Tinea versicolor diagnosis and treatment comparison - what the peer-reviewed science says.
If you’ve noticed light or dark patches appearing on your chest, back, shoulders, or neck—especially in warm weather—you may be dealing with tinea versicolor, a common and often misunderstood skin condition.
While it’s harmless, tinea versicolor can be persistent, confusing, and frustrating to treat without the right information. Understanding how it’s diagnosed and treated is the first step toward clearing it and preventing it from coming back.
What Is Tinea Versicolor?
Tinea versicolor (also called pityriasis versicolor) is a fungal skin condition caused by an overgrowth of Malassezia yeast. This yeast naturally lives on everyone’s skin, but in some people it grows out of balance.
When that happens, it interferes with normal skin pigmentation, leading to:
Light, dark, pink, or reddish patches, fine scaling, and mild itching (sometimes none at all)
It’s not contagious and not a sign of poor hygiene.
What Causes It?
Several factors make tinea versicolor more likely to appear or recur:
Hot, humid weather, oily skin, excessive sweating, hormonal changes, weakened immune response, and genetics could be at play.
Because the yeast is already present on the skin, treatment focuses on controlling overgrowth, not “catching” or “curing” it forever.
How Tinea Versicolor Is Diagnosed
1. Visual Skin Exam
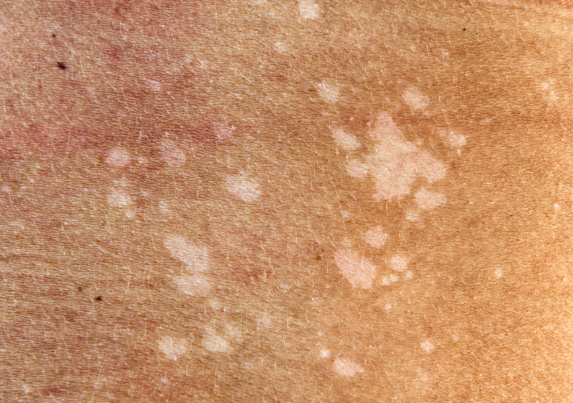
In most cases, diagnosis is straightforward. There is a lot of ways it can present and it looks different on different skin tones (see above) but in general you can tell if it’s textured and been around for a long while, it also likes to slowly spread. You can pretty much easily identify tinea versicolor just by looking at the pattern, color, and location of the patches.
2. UV Lamp Exam
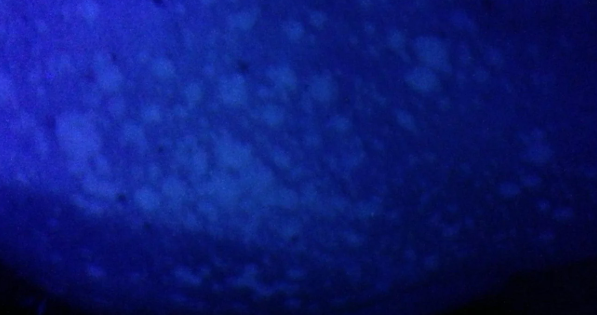
If you’ve got a UV lamp laying around or something in the black light family you might be able to see how the healthy and affected pigments contrast more effectively. Under this light, affected areas often glow signifying a lack of pigment where the melanin has been destroyed by the fungus. Kinda cool kind of a bummer.
3. Skin Scraping
In uncertain cases, a small skin scraping may be examined under a microscope to confirm the presence of yeast.
👉 Many people self-diagnose correctly, but seeing a professional is helpful if symptoms are atypical or persistent.
Treatment Options for Tinea Versicolor
Treatment works by reducing yeast levels on the skin. There are several effective approaches, depending on severity and recurrence.
🧴 Topical Treatments
These are usually the first type of treatment:
Antifungal shampoos (used as body wash):
Ketoconazole, Selenium sulfide
I’ve said it before and I’ll say it again, these often burn your skin.
Antifungal creams or lotions:
Ketoconazole, Clotrimazole, Ciclopirox, Terbinafine
These can work but peer reviewed studies show they’re not as effective as nitric oxide or acidified nitrite creams like TVT. (1)
✔ Easy to use at home
💊 Oral Antifungal Medications
For widespread or stubborn tinea versicolor, doctors may prescribe:
Fluconazole or itraconazole
These are usually taken for a short course.
⚠️ Oral medications are effective but require medical supervision due to potential side effects. I tried these to no avail and they made me feel terrible. Plus seeing a doctor and/or specialists is a totally unncessary step to treating Tinea versicolor. It’s much cheaper to take care of it yourself. You just need to pick the right product.
🌿 Natural Treatments
Some people prefer gentler or complementary options, especially for recurring cases or sensitive skin:
Tea tree oil (diluted), Sulfur-based washes
Apple cider vinegar (diluted)
Natural treatments may help control yeast growth but usually:
Work more slowly, require consistent use, and are best for recurring long term cases and maintenance
Why Skin Color Takes Time to Normalize
A common frustration:
“The fungus is gone, but my skin still looks blotchy.” This is normal. Even after yeast is controlled:. Light or dark patches can take weeks to months to fade. Sun exposure may make contrast more noticeable
This is a pigmentation issue—not active infection.
Preventing Recurrence
Tinea versicolor is known for coming back. Prevention strategies include:
Using a medicated or antifungal body wash periodically, showering after sweating, wearing breathable fabric, avoiding heavy, oily lotions on affected areas and managing heat and humidity exposure
For people prone to recurrence, maintenance treatment is often key.
When to See a Doctor
You should seek medical advice if:
The diagnosis is uncertain, symptoms don’t improve after treatment, the condition keeps returning, or if large areas of the body are affected.
A dermatologist can tailor treatment and rule out similar conditions like vitiligo, eczema, or psoriasis.
Tinea versicolor is common, manageable, and not dangerous—but it does require the right approach. With proper diagnosis and consistent treatment, most people can control it successfully and reduce future flare-ups.
Whether you choose prescription medications, over-the-counter antifungals, or natural support options, understanding how the condition works puts you in control. Let me know if you have any questions! Always happy to help.
All the best,
Your modern medicine man (and actual botanist)
Aaron
(1) Tirado-Sánchez, Andrés, et al. "Recurrent pityriasis versicolor: A short review of clinical features and antifungal and non-antifungal treatment options." Our Dermatology Online/Nasza Dermatologia Online 14.4 (2023).